Simple, everyday practices, including Aerosol Generating Medical Procedures and Events (AGMP&E’s), release infectious agents into facilities, resulting in blatant or occult contamination of the surroundings. Just one of the links in the Chain of Disease Transmission. Many studies have demonstrated that surfaces and medical equipment may harbour pathogens that can survive for extended periods of time (26). These disease- causing microbes can then be further mobilized when carried on a portable surface, such as a stretcher railing, IV cart, stethoscope, or personal protection equipment (PPE) worn by healthcare providers, or on their skin left exposed. The culminating concern is that patients, healthcare providers and support staff, equipment, visitors, and the entire institutions are constantly contaminated with mobilized pathogens that are becoming increasingly resistant to antimicrobials.
Current practices have been developed with a reliance upon pharmaceuticals, disinfecting products, hand washing campaigns, and PPE. Unfortunately, these previously effective approaches are no longer adequate to manage past HAI sources and outbreaks, let alone the COVID-19 pathogen overwhelming the globe piecemeal. Healthcare facilities continue to become contaminated with infectious agents and face an ever-increasing bio-burden of evolving pathogens.
Antibiotics have traditionally been successful at treating minor to significant infections since the 1940’s. However, the collateral and unintended impacts of these lifesaving medications on other common human microbes have resulted in the Anti- microbial Resistant Pathogen crisis that that has been growing steadily for decades. Front and center and attacking from without is obviously the predicted and so deadly COVID-19 or Corona Virus pandemic we are in. Broad overprescription of antibiotics has become the major contributor to the development of antimicrobial resistant bacteria (5). Recent studies indicate that 30% to 50% of antibiotics prescribed in ICUs in the US are inappropriate, unwarranted, or prescribed at sub-optimal doses (5). In many countries, the use of antibiotics is unregulated, used without professional oversight (1), available without prescription, and easily accessible on the web (5). With COVID the apparent disease transmission from an animal vector, perhaps bats, to humans makes it ‘novel’. That it has no preceding strain known to man makes it so deadly and untreatable.
Over the years, a great deal of research and funding has been directed towards disinfection of facilities through chemical treatments with fogs, sprays, lights, wipes, or other means. However, disinfection is seldom 100% effective as human error, among other factors, contributes to inconsistent or incomplete application. In addition, chemicals are sometimes associated with toxic or irritating residue and harmful fumes. Is the use of such potent cleaning actually a quiet and passive admission that the pathogen has been allowed to spread throughout the medical environment in the first place?
Hand-washing protocols, campaigns, and re-education have most likely mitigated the transfer of contaminants and disease transmission compared to any other single change in strategies in the past several years. PPE has long been considered the hallmark of infection control – the physical manifestation of infection control.
Healthcare workers (HCWs) rely most heavily upon the protection offered by PPE and it has become synonymous with the Infection Control. Unfortunately, there is a misconception regarding the degree of actual ‘infection control’ PPE provides. PPE can have unexpected failure and should not be relied upon solely to reduce the risk of exposure (20). Vast documentation and research surrounding the Ebola crisis has shown the effectiveness of PPE is questionable. It was reported that HCWs frequently self-contaminate when wearing gloves and gowns and contamination increases with a higher environmental bio-burden. The self-inoculated workers then “serve as vectors spreading the MRDO (multi drug-resistant bacterial organisms) to other critically ill patients if their hand hygiene adherence is not 100%” (9). In addition, healthcare providers do not clean their hands as frequently as they should. less than half the time than is recommended (8).
PPE provides some specific parts of the body, which is critical. However, PPE also offers a fleet of vehicle for the transmission of infectious agents. A study conducted examined the incidence of self-contamination by HCWs when removing PPE; 79.2% of wearers contaminated themselves (21). Another study focused on isolation gowns, which along with textile materials and other PPE, are known be a source of cross-infection (27). It is not unreasonable to extrapolate that the surfaces of PPE can transfer infectious agents to other patients, HCWs and the environment, thus expanding the area of contamination. In terms of worker exposure, blood, vomit, sputum, saliva, and urine make up the majority of sources of contamination (17). With COVID-19 aerosols seem to be implicated in the spread. Generally HCW’s report that their head and face are most frequently contaminated (17). These statistics are likely higher than reported as it was noted that most workers are not likely to report a splash on their uniform or face shield (17, 18). In every safety hierarchy portrayal, PPE ranks as the least reliable, least effective, least complied with, and most likely to fail of all interventions. PPE can contribute to the growing problem of AGPs and their resultant HAIs by playing the role of a reservoir and vehicle of transmission. It’s failure can also lead to HCW infection, treatment with antibiotics and furtherance of the potential for more resistant ARP’s.
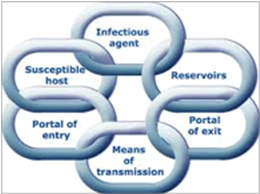
The chain of infection is a model used to describe the transmission of disease (Figure 1). In general terms, the healthcare system has directed control measures towards the link in the chain which most easily lends itself to intervention, often budgetary restraints or tradition being the determining consideration. Efforts have been, and continue to be, focused upon eradication of the infection from its host source with interventions including antibiotics or interrupting the transmission of the infectious agent. Other approaches include protecting portals of entry in hosts through mechanical aids such as masks or a potential host’s internal defense with vaccines.
These measures have simply been inadequate in halting the persistent, invasive progress of occult and dynamic infection. The situation has become more a game of infection chase rather than infection control. Now of course the game has been upped since we have neither pharmaceutical treatments, inherent antibody facsimiles and a highly transmissible pathogen whose arrival symptomology may not be announced to the new host for days. In the world of healthcare workers this means they could be contacting and unknowingly infecting a far greater percentage of more susceptible potential hosts than the average slice of society.
Note: This document has been edited. Original text and references can be found on the original document on our website www.prodaptivemedical.com.

